PECs Nerve Block
Until recently, patients having anterior chest procedures involving the pectoral muscles such as breast reconstruction had only two regional anesthetic choices for intraoperative and postoperative pain control. These included the thoracic epidural and, more commonly the thoracic paravertebral block. Since many of these reconstructive cases are done on an outpatient basis, the epidural approach is considerably less desirable and may pose significant risk to the patient. The alternative approach for analgesia pertaining to outpatient breast reconstruction cases is the thoracic paravertebral block (PVB). While less risky and having a longer duration, it is often less than effective in producing the desired analgesia. The reconstructive breast procedures have considerable pain arising directly from the pectoral muscles themselves. This can be because many surgeons find it desirable to place breast implants under the pectoral muscles. This produces pain and pressure sensations by the pectorals. Spasm of the pectoral muscles during the immediate and more distant post operative period is also an issue that patients and surgeons struggle with. The pain response from the pectoral muscles, not the skin, fascia and mammary tissue, makes the thoracic PVB less or ineffective for reconstructive cases. This is sensible because the block essentially doesn't match the surgery. The likely reason for this fact is that the pectoral muscles simply aren't innervated by the spinal afferents carried under the ribs.
A new procedure targeting the innervation of the pectoral muscles for breast reconstruction has recently been explored. This new approach is called the median and lateral pectoral nerve blocks. This approach is safe, simple and effective- although it is so new it hasn't been investigated to any great extent. This novel approach takes advantage of the superficial nature of the target nerves and no requirement to image the nerves themselves. The pectoral muscles themselves are superficial structures and image well with even poor ultrasound equipment.
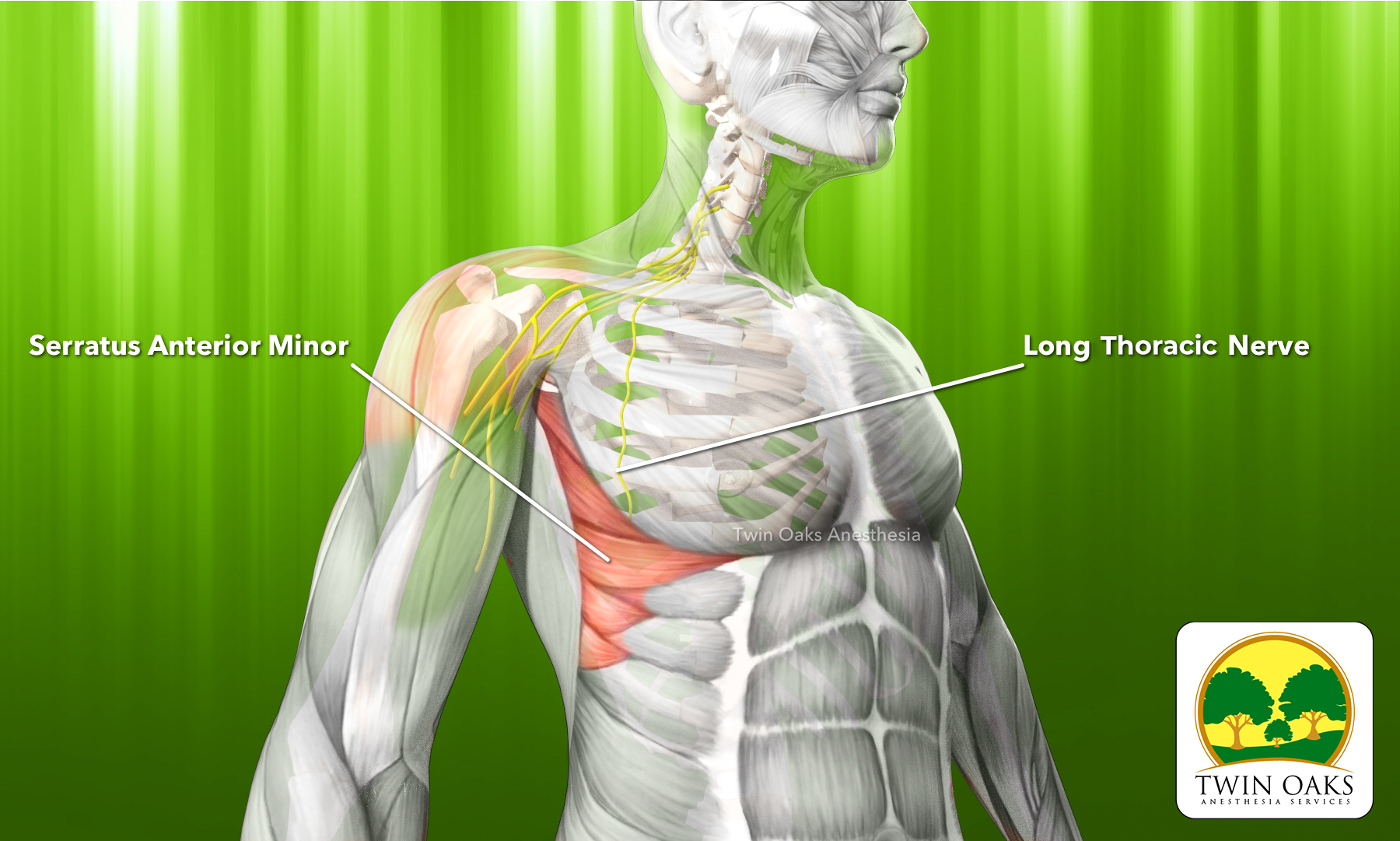
The block involves both the medial and lateral pectoral nerves. The median pectoral nerve arises from the brachial plexus. Specifically the medial cord of the plexus. It derives spinal contributions from C8-T1. After leaving the plexus it runs between the pectoralis major and the pectoralis minor muscle. It sends off about three additional branches into the pectoralis major muscle as well.
The lateral pectoral nerve arises from the lateral cord of the brachial plexus. It derives spinal contributions from C5-C7. It leaves the brachial plexus and also runs between the pectoralis major and minor muscles. It innervates solely the pectoralis major muscle. The path that these two nerves share is the space between the pectoralis major and minor muscles.
The performance of any block begins with a proper patient and block selection, full explanation and disclosure of the risks and benefits, institutional procedure for laterality and time-out. Contraindications would include patient refusal, infection at the site and allergy to local anesthetics. Caution should be used for any patient receiving a peripheral nerve block while in a state of anticoagulation.The technique for blocking the medial and lateral pectoral nerves essentially is a hydro-dissecting field block that has been described under ultrasound guidance. The procedure for this block directly follows the anatomical description of the nerves running in the plane between the pectoralis major and minor muscles. Begin by noting the correct block side and position yourself on the opposite side. Assemble all necessary equipment, obtain consent and sedate the patient with standard monitors. This will allow for needle guidance away from the chest. Position the ultrasound monitor on the same side as the block. A high frequency linear probe is selected and set to a depth of about 2-4 cm. Muscular males may require deeper settings to penetrate enlarged pectoral muscles. Place the probe under the clavicle as if doing a infraclavicular procedure. Optimize the image to allow for visualization of the junction of the pectoralis major and minor muscles. This image should show the large pectoralis major muscle superficially and smaller/thinner pectoralis minor muscle deep to it in short axis. You should also note the placement of the subclavian/axillary vessels. Rotate the probe to produce a long axis image of the pectoralis group to allow for needle guidance away from the chest. Administer a generous amount of local with a small needle such as a 25 gauge to awake patients. After skin localization, guide a blunt tipped needle, using an in-plane approach, to the site of the thoraco-acromian artery, which lies in the junction between the major and minor muscles and aspirate. This should appear as a hyperechoic line defining the two muscle planes. A trick to finding this plane is to simply move the elbow up and down while watching the monitor. These two muscles will appear to move against each other, accentuating the plane. Upon negative aspiration, hydro-dissect the space to both both nerves. Caution should be observed not to place the local into the muscle bellies. This will likely lead to block failure and more rapid absorption of local anesthetic. Volumes of 10- mLs of local anesthetic has been described although this needs further investigation. A perineural catheter can be easily placed after placing the bolus dose, however care must be taken to stay clear of the surgeons field during the procedure. . This will likely facilitate a smoother catheter placement. If this technique is used in conjunction with a thoracic PVB a reduction in bolus dosing is recommended (by this author) as total dosing for both blocks can easily exceed safe levels. This is particularly important when considering the relatively thin patient requiring a bilateral mastectomy and reconstruction. These procedures are often done separately, but dosing regimens are important to keep in mind. For a fairly complete block for a combined mastectomy and reconstruction, consider omitting the bolus dose for the pectoral block and place a slow dosing catheter at about 5 mLs per hour to each surgical side.
This image shows the relevant anatomy for the PECs 1 block. Note the appearance opf the pectoralis major on top, and the pectoralis minor below. the plane is interrupted by the thoraco-acromian artery.
We hope that you'll find the procedure notes provided on this site useful. They are designed to provide you with the essentials to make your documentation easier and more complete. Please feel free to copy and paste the language provided and modify/customize these forms in accordance with your institutional policies. It should be noted that we in no way intend these to be used in their exclusive entirety, take no liability for any performance of any procedure, or responsibility for content that is modified. They are to be used to provide you with a foundation, for which to build your own procedure forms and are not intended to be used unaltered.