Erector Spinea Nerve Block
As surgeries of the trunk, from thoracotomy to plastics procedures or the chest and abdomen , are on the rise, as is the need for pain control for these areas. For decades thoracic and lumbar epidural techniques seemed to offer the only viable solution. However their drawbacks and limitations often make them unsuitable or simply too risky for anesthesia providers to employ. This need for effective chest and abdominal wall analgesia has therefore stemmed a few emerging alternatives such as the PECS series, thoracic paravertebral blocks and the targeted TAP procedures. But recently a simplified version for providing anterior chest and abdominal wall analgesia has been described. This relatively new technique is termed the erector spinea (ESP) plane block.
The erector spinea (ES) block takes advantage of the previously poorly described and understood anatomy of the paraspinous region. Although the bony structures in this area are well described, the blockade of channels that contain the sensory innervation, particularly the cutaneous nerve tracks and gutters connecting various regions is not well understood. In comparison to similar techniques such as the paravertebral block, quadratus lumborum (QL 1,2,3), and serratus anterior plane block, this variation seems to hold promise. But this leaves practitioners wondering what the mechanism of action really is, and why all these variations of the block seem to be equally effective. This paves the way, based on our current understanding, that it doesn't seem to matter where these techniques are placed, but that they all have the capability to cover similar regions and dermatomes. Another area of interest regarding these blocks is that unlike the previous postulation that local spread deposited more centrally, between specific layers would spread laterally, these newer techniques have shown to remain in the paraspinous gutter. Another exciting notion is emerging from the literature regarding these more central blocks, is that blockade more completely covers not only cutaneous branches, but visceral branches as well. This notion may prove to be quite valuable as the anesthesia efficacy for deep pain may actually be accessible outside the neuraxial space. This would be a significant step forward in anesthesia safety and allow for a much wider inclusion of patients, who would not be suitable for central neuraxial techniques, such as patients on anticoagulants. Lastly this, and related techniques have suggested, by virtue of all of them proving efficacy, that there may be communication between these various layers of posterior thoracic musculature, allowing local anesthetic access to all these nerves, as they pass through these previously not appreciated pathways.
Indications for the block are constantly being evaluated. Literature seems to support the typical block success for breast, chest, and abdominal incisions. Some scant information reveals that some somatic and visceral coverage is possible with this block- a distinction shared only by its classmate the quadratus lumborum block.
ANATOMY
The term "erector spinea” is a name of convenience. There is no muscle called the erector spinea, rather its a description of a muscle group performing the action of “erecting the spine”. These muscles in the group are the iliocostalis lumborum and the longissimus thoracis. The block focuses on the relationship of the three superficial layers of the peri spinous musculature and the dorsal rami contributions from the spine. These cutaneous branches that innervate not only the skin and subcutaneous layers of the back but also the anterior chest. Previously it was thought that these nerves that leave through the neural foremen and travel through the paravertebral space were only accessible by violating the paravertebral fascia. However it seems that channeling exists connecting these regions of the posterior musculature. The midline layers of musculature are the latissimus, rhomboids and the erector spinea muscles. These layers seem to form a continuous channel from the lumbar to the cervical spine that previously hasn't been well described or utilized. It's an important caveat that the anterior chest wall musculature of the pectoralis major and minor are exclusive of this list, as is the region of the sternum.
Technique
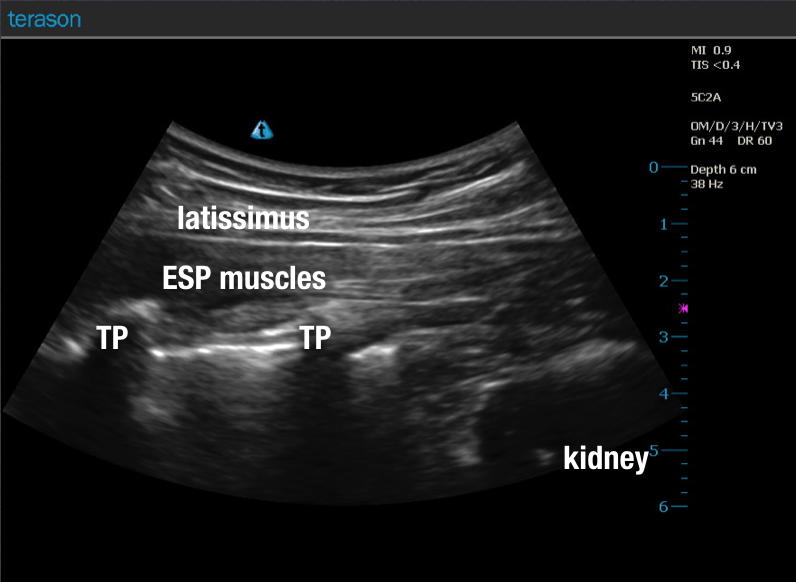
The technique has been described with a few variations. It does however seem pretty universal the the needle should be guided under ultrasound imaging. Various articles describe using the linear probe but the the curved probe is also indicated for obese and relatively deep needle trajectories. Since the goal of the block is to place local anesthetic under the erector spinea and above the transverse process, it seems sensible to obtain an axial view of the spine, and isolate the transverse process. See gallery 35.1 for images. One such description includes beginning the scan by first getting a transverse view that includes both spinous and transverse process at the level of surgical incisional interest.
Once the transverse process of interest has been identified, the probe is then repositioned in a longitudinal (axial) fashion, to include the tip of the transverse process, and three layers of the peri spinous region. Early work has demonstrated that a single injection at the level of T-5 may spears axillary from T-1 through T-8. The view should include the dorsal musculature in two to three layers and the transverse process. This will depend on the spinal height of the target region. After skin and drape (per institutional policy) the skin and projected needle path should be localized with a fast acting local such as lidocaine 1%. This reduces patient discomfort and increases image quality by harnessing acoustic enhancement. A block needle is the introduced in plane to contact the lateral tip of transverse process. The direction of cephalad to caudad, and caudad to cephalad have both been described with success, so it seems that the needle direction is not of great importance. After negative aspiration, local is deposited under the erector spinea muscle. Careful attention should be paid during initial deposition as misplacement into the muscles is not desired. Additionally, the displacement of the erector spinea group superficially from the transverse process is a good indicator that the local has been properly placed. It seems that 20 cc has been most popular volume described by authors per injection side. However, modifications can be made to tailor the prescription to match the clinical situation and block goals. Successful posterior (superficial) displacement of the erector muscle and anechoic stripe connecting the adjacent transverses processes seems to be recommended and included in the various articles available. Many articles state that the block at 20cc does not seem to last long. The addition of dexamethasone seems sensible to extend block duration. Additionally, if the ESP block is done in combination with other block techniques such as tumescent fluid of a myriad of other regional techniques is done, the addition of epinephrine can delay uptake, and may also reduce the serum concentrations of long acting locals like marcaine or ropivacaine. A few of the articles have done single shots to prove success followed by catheter placements for continued analgesia. Since rapid onset is usually not the goal in conjunction with other anesthetics for surgery, a fast local nor high concentration local is needed. It seems logical that a low concentration, long acting local such as ropivacaine in a volume of 20 cc for adults be used as a starting point. As motor blockade is noit a goal of this technique high concentrations of any local is not needed to achieve block success. This may further increase safety margins and allow for increases in volume in other areas.
We hope that you'll find the procedure notes provided on this site useful. They are designed to provide you with the essentials to make your documentation easier and more complete. Please feel free to copy and paste the language provided and modify/customize these forms in accordance with your institutional policies. It should be noted that we in no way intend these to be used in their exclusive entirety, take no liability for any performance of any procedure, or responsibility for content that is modified. They are to be used to provide you with a foundation, for which to build your own procedure forms and are not intended to be used unaltered.